17 Common Myths About Acne You Should Stop Believing
Sherry Haynes is currently pursuing a PharmD degree and has experience in both the clinical and management sides of pharmacy.
Acne is one of the most treatable skin disorders. But it is shrouded by myths that stand as a barrier to its treatment. Patients turn to the media for medical knowledge and those with a poor understanding of the disease continue to spread the misconceptions. For people with acne, these misconceptions contribute to skin problems, leading to complications like scarring.
1. Acne is a trivial condition and does not require medical attention
Most people have only a mild form of acne, hence it is viewed as an insignificant condition. However, this cannot be further from truth. Even though the physical symptoms—including itching and pain—are minor, acne is associated with anxiety, depression, and embarrassment. More than 70% of people who have acne wait for more than a year to seek medical attention and most of them choose to seek care in beauty salons.
If left untreated, waiting for the natural healing to occur, acne can develop into nodules and cysts. These lesions leave scars. Nodules, cysts, and scars can cause psychological stress.
Acne should be treated as soon as it occurs before the complications set in.
2. Acne should disappear by the end of adolescence
Many people seem to think acne is a disease for teenagers and will wear out with time. The truth, however, is that the prevalence of acne is highest in teenagers due to increased androgen secretion and sebum production. Acne does clear up in the twenties because the pilosebaceous ducts do not react to hyperkeratinisation to androgens after some time. Nonetheless, acne may persist well past adolescence. A German study found that 64% of patients were affected by acne in their 20s. Moreover, 43% and 24% of patients had some degree of acne in their 30s and 40s respectively.
3. Acne is caused by uncleanliness
There is no link between facial cleanliness and acne. The numerous facial regimens marketed out there are only expensive face washes with no clear evidence showing efficacy.
Moreover, frequent face washing can be traumatizing. It removes sebum from the skin's surface making it dry and irritated, which can exacerbate acne.
Dermatologists have suggested that irritation from frequent face washing may lead to nonadherence of topical acne medicines, resulting in poor clinical outcomes.
4. Acne improves rapidly upon treatment
The advertisements for an overnight cure can be tempting, but those are advertisements for a reason. Acne is a slow-responding disease, and even the most effective treatment program may take 4–6 months to show improvement.
Most patients are not willing to take antibiotics even in the initial months and then stop taking any medicines. This is the most common reason for treatment failure.
5. Sunlight and tanning help acne
Even though recent findings have suggested that artificial light is efficient in acne treatment, this may not be generalized to natural sunlight. Long-term UV light can be carcinogenic. Visible light may be relatively mild and useful. It stimulates the natural porphyrins produced by bacteria. Blue light and light of longer wavelengths may kill bacteria, lessening the disease. Similarly, photodynamic therapy is used with exogenous porphyrins.
Additionally, if you are taking tetracyclines (a class of antibiotics) or isotretinoin, photosensitivity, a side effect of these medicines, is an issue.
6. Scrubbing the face daily clears up acne
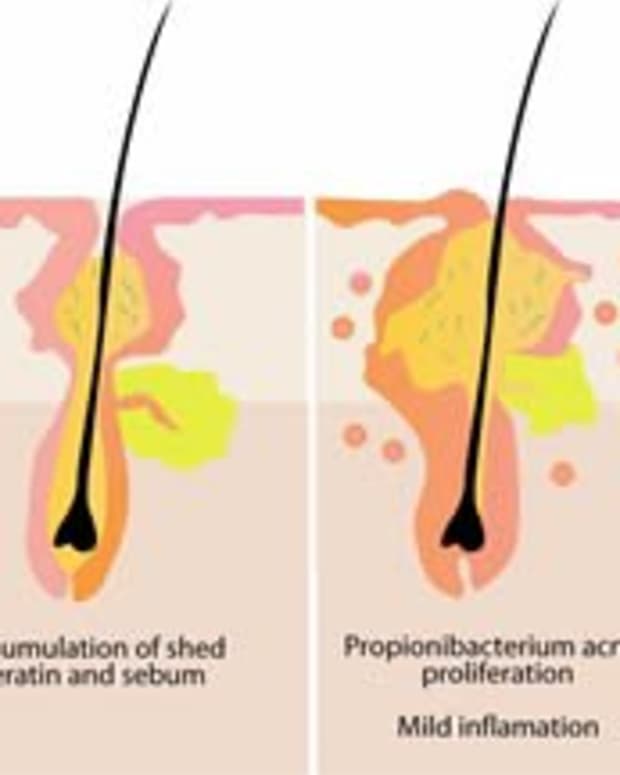
Excess sebum is produced in most acne patients. But, this surface oil is not dirt. Though it is true that sebum blocks the pores, contributing to acne. The pores are at a depth well beyond the washing techniques. Scrubbing does nothing to help clean the pores.
Scrubbing and rubbing the face, particularly in inflammatory acne, irritates and reddens an already inflamed complexion. Instead, the face should be washed daily with gentle cleansers.
7. Acne is contagious
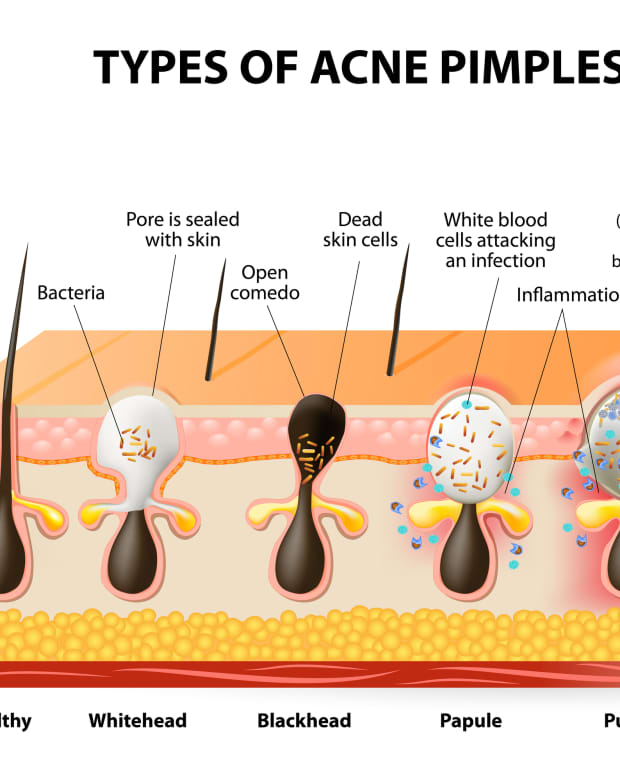
Some people believe that they are infectious to others. It may be because of the involvement of P. acnes bacteria in the disease. It is true that the bacteria promotes the extension of acne from micro-comedones to fully developed inflammatory lesions but this happens only after acne has been initiated. The bacteria live deep inside the pilosebaceous apparatus and dies when coming in contact with air. So, there is no chance it can wash away from the surface to another person.
Another reason people seem to think acne is infectious is the use of antibiotics for the treatment. But in acne, the antibiotics are prescribed for their anti-inflammatory effect besides their bactericidal effect.
Read More From Bellatory
8. Acne is curable and a course of antibiotics is all that is needed
Acne cannot be cured, although Isotretinoin may cause long-term remission of the disease. Continued treatment is required in most cases.
9. Taking vitamin A orally may help acne
I have to admit that this was one misconception to me. I thought that because vitamin analogues are helpful in treating acne, oral vitamin A should help likewise. Vitamin A can be effective but in toxic doses. Isotretinoin is much more effective and comparatively safe.
10. Acne is a symptom of pregnancy
Some women see improvement in acne during pregnancy or while taking birth control pills. Others may note the worsening of acne or no change at all.
11. Moisturising and frequent facials help acne
Moisturisers, masks, facials, and astringents have no value in treating acne. They usually worsen the acne and should be avoided.
12. Cosmetics cause acneiform eruptions
This was a fact a few years ago. There were cosmetics containing comedogenic (acne-causing) substances such as Isopropyl myristate. However, most cosmetics today contain non-comedogenic products and are usually safe.
13. Blackheads are black because of dirt
Blackheads are black because of the oxidization of melanin. Blackheads (medically termed open comedones) are a collection of sebum and keratin within follicular openings. When exposed to air, melanin become oxidized and turn black.
14. Infrequent shampooing or long hair predisposes one to acne
Infrequent shampooing, leaving the hair long, greasy hair, or wearing the hair over the face does not predispose one to acne. However, one study suggests that excessive combing and brushing of hair may exacerbate acne.
15. Medications should be applied topically only on spots
The topic treatments including cream, ointment, and gels should be applied to the entire affected area, not only on the spots. There are micro-comedones present on the skin which are invisible to us. But these can develop into bigger lesions. So, to prevent them from developing, the treatment is applied to them.
16. Acne lesions can be squeezed
Popping the acne lesions by squeezing may make the lesions less visible temporarily. But this may be followed by severe inflammatory lesions in a few days. Squeezing causes the rupture of the pilosebaceous duct. The contents pass into the dermis where more inflammation takes place, resulting in a deeper and severe reaction.
17. Sunscreen clogs acne pores
When exposed to the sun for longer periods of time your skin can dry out, causing acne flare-ups. Plus, acne medicines can cause photosensitivity. Sunscreen protects the skin from damaging infrared heat. However, you need to find the right sunscreen as most of them are too oily and can aggravate acne.
Sunscreens with physical blockers such as zinc oxide and titanium oxide are greasy and have large particles that can block the skin pores.
Even chemical sunscreens can be good or bad. Spray or gel-based sunscreens with microfine particles are best for acne-prone skin.
Further Facts
- No direct link has been found between acne and diet. Studies are underway but there is no scientific-based evidence suggesting any clear link. High glycaemic food including dairy products, sugar, white bread, and white rice have rich carbohydrate content and are rapidly absorbed, leading to increased serum glucose levels and corresponding elevated insulin.
- Insulin and Insulin-like growth factor-1 (IGF-1) increase serum production, stimulate androgen synthesis, and increase androgen bioavailability. All of these play a role in acne improvement. This theory was tested in two trials, both of which showed improvement in acne and insulin sensitivity.
- Chocolate and similar foods may increase blood lipid levels, which can produce more comedogenic sebum or it may produce less-fluid sebum—both of which cause obstruction of pilosebaceous glands, exacerbating acne. Neither of these two mechanisms can produce a change in a short time frame.
- Teenage acne is much more likely to be hereditary and less likely to be seen in Asians and dark-skinned people.
- In most people, acne improves temporarily during the summer months. Little exposure may diminish acne and tanning products promote blending of the skin tone.
- Acne, hirsutism, and irregular periods may be linked with hyperandrogenism or polycystic ovaries.
- In dark-skinned people, the severity of inflammation may be equivalent to that of fairly skinned people. But it may not be as apparent.
- Stress cannot cause acne but can worsen it. Stress has an effect on hormones.
- Some drugs like lithium, steroids, epilepsy drugs, and antitubercular medicines, can cause or exacerbate acne.
- Sweating or a humid environment may cause acne.
- Weight loss and acne: Weight loss and the use of metformin (an antidiabetic medicine) are both associated with lower levels of insulin and androgen. IGF-1 levels are reported to be elevated in acne. Through a similar mechanism as explained earlier, with hyperinsulinemia, there may be increased androgen production, resulting in increased stimulation of sebaceous glands. This might be the case in obese acne patients.
Before undertaking any treatment, proper education about the disease, how it occurs and progresses, and the likely outcome should be known.
References
- A systematic review of the evidence for ‘myths and misconceptions’ in acne management: diet, face-washing and sunlight
- Common misconceptions about acne vulgaris: A review of the literature
- Sunscreening Agents
- Diet and Dermatology - The Role of Dietary Intervention in Skin Disease
- Dispelling the Myths and Misconceptions of Acne
This content is accurate and true to the best of the author’s knowledge and is not meant to substitute for formal and individualized advice from a qualified professional.
© 2018 Sherry Haynes